 |
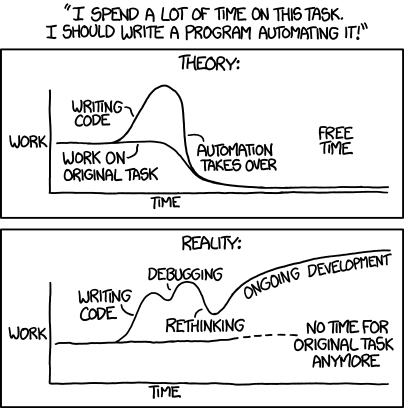
| XKCD for Jan 20, 2014 |
It ruffled my feathers a bit; automation is a big part of what we do for clinical labs and I know, I can prove, that we leave processes faster, cheaper and better when we are done with them.
This is, in part, because we go easy on the "rethinking" part. We like business process engineering, the careful defining and describing the working parts of a process as though that process were a machine. Through careful description comes understanding.
We fear business process re-engineering, the long and tedious process in which MBAs and frustrated worker bees compete to imagine a perfect world which software people are then to summon from the ether.
We understand that the pieces interact and interconnect. We also understand that predicting how it will all shake out is a very low-percentage business so instead of trying to fix the entire process, we go after low-hanging fruit and iterate.
Billing wants paper from which to work? Fine, give them cheap, simple reports and print them. Once they believe in the reports, they may be open to a web page instead of printing. Once they trust the web page, they be willing to consider a data feed. Once they have the data feed, who needs all this damned paper?
"Please stop printing those reports, nobody looks at them any more" is how our successful automation gigs end. But we don't start with "you guys need to ditch the paper, this is the 21st century!"
The clinical lab was slow to embrace automated analyzers and autoverification, but embrace them they did. The greying of workforce and lack of new blood means that it is time to take the automation behind the bench.
We know that some IT "automation" made data entry and other tasks slower and harder, but please don't tar us all with the same brush: there are plenty of tasks the computer can do faster and better, so you can concentrate on the other stuff.
.svg/140px-Great_Seal_of_the_United_States_(obverse).svg.png)




 AWS enables covered entities and their business associates subject to the
AWS enables covered entities and their business associates subject to the